Mind the covid-19 mutation gap
Key points addressed in this article:
1. An explanation of the reason why respiratory viruses such as covid-19 can be deadly.
2. Why the broad region of Oceania had very little mortality during the early stages of the covid-19 pandemic.
3. Why vaccines can have positive and negative impacts.
4. Why respiratory viruses become less deadly with time.
5. Why we are seeing significant excess deaths.
6. Why Sweden did well in terms of excess mortality during the pandemic period.
The proposed hypothesis is relatively simple;
Respiratory viruses, such as covid-19, continuously mutate as this is essential to their survival. Respiratory viruses initially embed in a population at a low level and only have a serious impact, in terms of severe disease, when a mutational gap has emerged and the mutated virus is transmitted to individuals who are significantly less healthy than the originating hosts. Less healthy in terms of this hypothesis is the specific response to that specific mutation. If individuals are exposed to relatively small steps of viral mutation, then immunity is induced with relatively minimal serious impact. There is nothing new about this concept as it has been widely acknowledged that the Incas were dramatically impacted when the Spanish conquistadors introduced new mutations of pathogens, such as small pox and influenza, to an immune naïve population.
Expanding on this concept with respect to the points above:
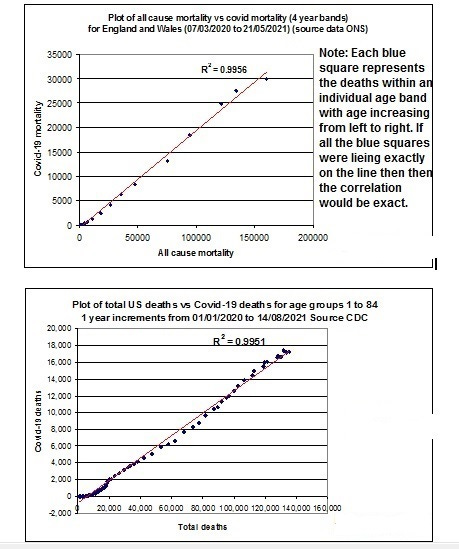
1. The most influential factor in terms of serious disease and mortality for covid-19 has been age. As people age, they suffer from immunoscenescence, which is a decline in their immune system. When such individuals are exposed to mutations that have escaped “healthy” systems the impact on the aged and the “unhealthy” is accentuated as the viral immune gap is significant. Further evidence can be seen of the impact of age and general health can be seen if we plot covid-19 mortality versus “normal” mortality we get a straight line. This indicates that covid-19 mode of mortality correlates strongly with the general health risk of the population.
2. One of the most notable aspects of the covid-19 pandemic was that the general region of Oceania had very little impact in terms of mortality. This was probably due to the virus originating in this region and for at least one season circulated widely. During this period the virus mutated steadily and there were limited viral mutation gaps. The population was effectively building steady herd immunity. Viruses require a host to replicate and therefore mutate through replication errors. Covid-19 embedded at a low level and it is not until there has been significant replication that more pathogenic mutations occur. Effectively the human immune system is filtering more transmissible variants that can evade the prevailing immune status. Due to global travel the mutated virus spread around the world to more naïve populations and therefore had a much greater impact. This impact was magnified by seasonal activation of covid-19. I have explained this concept in depth in previous articles but essentially it a seasonally activated mechanism for selecting mutations that can evade the prevailing state of the human immune systems (1). Consequently, if there are large seasonal and therefore viral mutation gaps, such as between Oceania and Europe / USA / South America, a more dramatic mortality event can follow.
3. Respiratory viruses become less deadly with time as immunity is built up within global populations. The virus has less and less successful mutational options that have the capability to escape the prevailing global immune condition. The variants that can escape have diminishing variation, so the viral mutation gap is reduced, and the severity and lethality follow suit. We have seen this with the emergence of Omicron as the dominant / highly transmissible but less lethal variant.
4. Various researchers have identified that vaccines, such as those for influenza, can have positive and negative impacts (2,3,4). A possible explanation is that we have to guess the circulating influenza virus to create a vaccine that can potentially induce an appropriate immune response. If we get it right a positive effect on mortality is observed but if we get it wrong, we redirect the immune system to create an immune gap with more severe consequences.
5. The above hypothesis could explain why the current vaccine program is having increasingly negative consequences. This was a relatively new virus with a significant mutation rate. If we inject with any “vaccine” designed to create an immune response specific for a previous variant, then we could be redirecting the immune system to create a viral immune gap. If you continue to inject on past variants this viral immune gap will increase in terms of infections specific to covid-19. Since many viral and bacterial pathogens exist in a relatively latent / low level state within our bodies the impact of continual frequent vaccination may be more diverse and result in mortality from other causes. It is probable that the excess mortality, that has been seen on a global basis, is multifactorial.
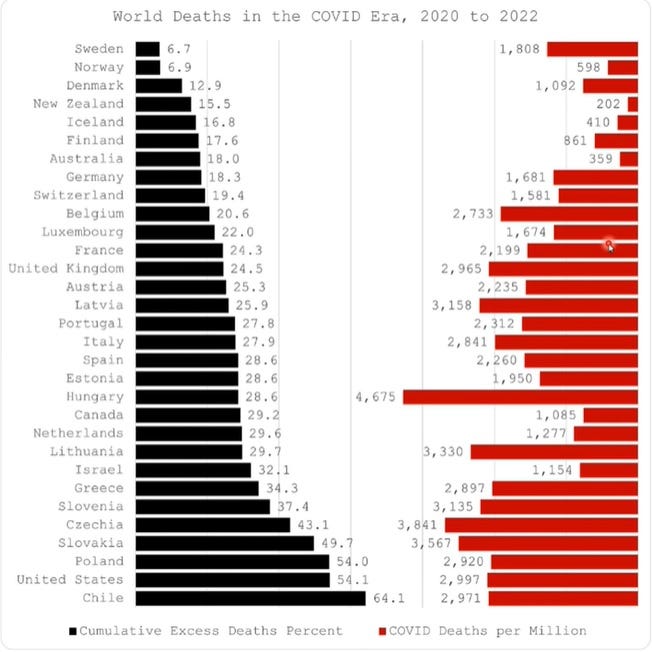
6. If this simple hypothesis is correct, then the implications are significant. The measures that were implemented virtually on a global basis would have, if anything, a negative impact in terms of the severity of impact of covid-19. This is because if they are effective they have the potential to create viral mutation gaps. Currently the best option is to let pathogens circulate and where possible build steady ongoing immunity. Which seemed to be the original WHO policy but was abandoned during the pandemic panic. The excess mortality data for different countries support this concept as Sweden allowed steady circulation during the pandemic period;
References / links:
(1)
(3)
(4) The non-specific and sex-differential effects of vaccines | Nature Reviews Immunology